START YOUR JOURNEY WITH EBPA
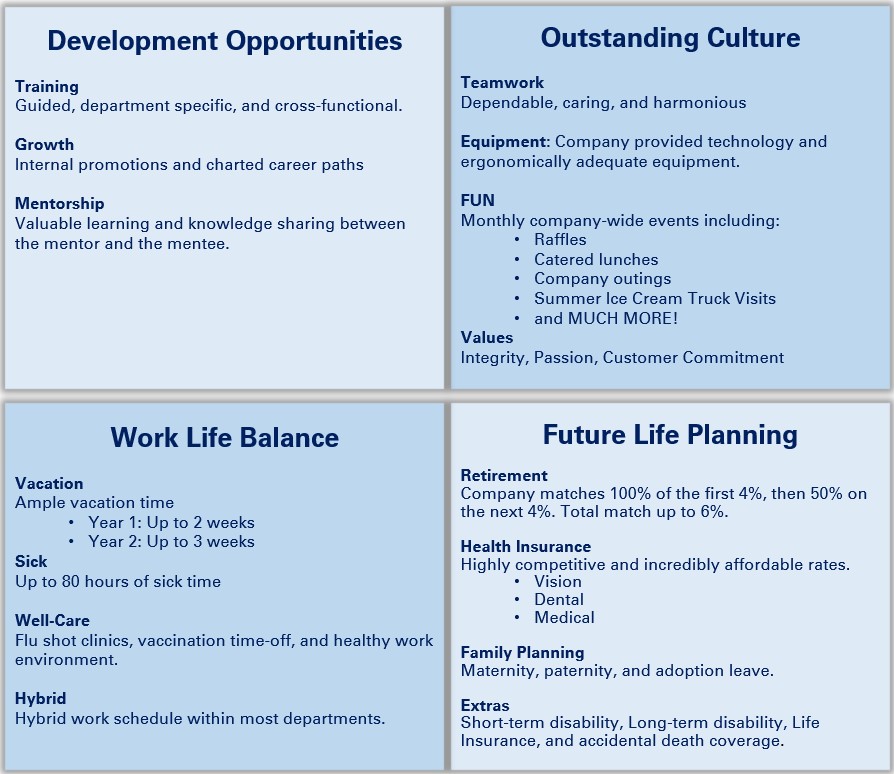
Here at EBPA, we understand that providing and maintaining a successful, long-lasting partnership with our members and clients starts with our own employees. Our employees are vital, and the foundation to providing superior service to all our members and clients.
READY TO JOIN US?
Current Job Openings. Don't see a job posted? Send us your resume and cover letter and maybe we can find a fit! We are always growing and always searching for new talent to join our team.
Check us out on LinkedIn